Productivity Indicators in Public Hospitals
(*) Medina, Orlando Francisco; (**) De Marco, Myriam Lilian Cecilia
(*)Facultad de Ciencias Económicas
Universidad Nacional de Tucumán
San Miguel de Tucumán – Tucumán – Argentina
omedina@face.unt.edu.ar
(**) Facultad de Ciencias Económicas
Universidad Nacional de Tucumán
San Miguel de Tucumán – Tucumán – Argentina
mdemarco@face.unt.edu.ar
Reception Date: 06/02/17 - Approval Date: 20/05/2017
ABSTRACT
The public hospital is the great receiver for excellence in what refers to trauma, but this excellence seems to fade to bad building conditions and inefficient processes, product perhaps of the imposing current message stating that public health must be just for the indigent, acting as an indigent hospital itself.
This research deals with the analysis of efficiency of this non-profit entity based public health sector indicators as a useful management tool. It was determined that the result of the activity of the public hospital as a nonprofit entity usually not a tangible output, but the fulfillment of objectives in providing a range of services to the community. The contribution of these social welfare would be the ultimate point of reference to guide the allocation of resources designed to meet the needs of the population.
The aim of this work is to develop management indicators from an internal and external perspective that will allow the achievement and monitoring of the strategy, and consequently improve the health service. This matrix of indicators allow to present the reality of the institution at a given time.
This article presents specific indicators of hospital management related hospitalization area, as part of developed control box.
KEY WORDS: Indicators; Management; Productivity; Hospital; Internment.
INTRODUCTION
The new public management involves moving from the concept of managing (following instructions) to managing (achieving results), which requires the use of control techniques that verify the achievement of objectives.
In this sense, hospitals have to adapt to the demands of this time, to social, political and economic externalities and to changes in their basic structures, tending towards a modernization that allows them to focus on their essential competences, integrating knowledge with the efficiency in the use of resources and the increase of equity.
The new hospital management needs to have information to make decisions. Hospitals generate a lot of data from different sources, but this information, although sometimes it is usually accessible, has little use in management. There are several reasons for this underutilization: the information that most interests clinicians is usually immersed in a broad set of data of little interest to them; the indicators are complex, they are generated at different times and, if they are not disseminated properly, they do not reach all the people involved in the management.
The joint analysis of what we could call strategic management and performance evaluation has been definitive in terms of obtaining adequate management results. Precisely, one of the tools that perfectly combine these two concepts is the integral control panel or integral command board.
The balanced scorecard is an integrated, balanced and strategic way to measure current progress and provide future direction, allowing to transform vision into action through a coherent set of objectives and indicators.
This scorecard applied to the public sector has the following features: non-financial perspective (in terms of profit); greater importance of performance measurement; reduction of inefficient operating costs; success is measured in terms of efficiency and effectiveness in satisfaction of users.
In this research we were interested in focusing our attention on the evaluation of the performance of the hospitalization area of a public hospital in the Province of Tucumán.
DEVELOPMENT
New models of hospital Management
Hospital management model Hospitals are service organizations that fulfill an essential social function, for what they need to develop a management that, listening and understanding the phenomena that make up the environment of the organization, know how to identify and project to the needs of its users who always have a different tomorrow.
Hospitals need to be more effective and efficient, closer to the people they serve, more open to citizen participation, to social control, more sensitive, flexible and dynamic in adapting to the needs of individuals and communities. This requires profound changes, especially because public hospitals are rigid and bureaucratic, with heavy and vertical structures, with legal and centralist limitations in the management of financial and human resources, and with a culture that is not very sensitive to the needs of people and changes in the environment.
For this reason, for the legitimation and development of public hospital organizations, maintaining a permanent and complex process of adaptation is an unavoidable necessity, since health care services must be in permanent adaptation with respect to to the changing health needs of people and communities, the changing expectations and cultures of the users of services, new technologies, both clinical and management, new models of organization and management of health systems, new possibilities of financial instruments and forms of financing, and the changing aspirations of personal development and creative contribution of the members of the organization.
Thus, the fundamental thing to legitimize and maintain in a dynamic environment, is that hospitals develop the capacity to change intentionally and continuously; Therefore, what is critical for the construction of the new hospital is the ability to learn to change, or what is the same: the institutional capacity to learn to listen and understand.
Given this new scenario, a new model of hospital organization is essential, configured as a living and open system, clearly influenced and projected to the values of the people who make up the organization and its environment.
New models of hospital organization
The situation of Provincial public hospitals was critical in three fundamental aspects: efficiency (in low productivity and reduced overall efficiency); quality of care; and limitations in the accessibility to health services for the poor population.
The daily work of the traditional public hospital was given by a culture of administrative management based on rejection of risk, a low level of motivation and a great weight of the bureaucracy, which generated a model of continuity management, with excessive centralization and low levels of autonomy, very regulatory, and with great difficulties for the introduction of new management instruments. Given this context, a new management approach is proposed with the main goals of increasing productivity, efficiency, quality of care, coverage and equity of hospital services. In order to achieve these goals, it is necessary to incorporate a business management model based on strategic thinking, great autonomy and commercial orientation into hospital management, even if this is public and without profit motives. [From Marco and Medina, 2012, p. 3]
In summary, from the traditional hospital environment it is necessary to move to a business environment - hospital as a service company: quality and efficiency - with clearly differentiated premises, in which risk appears in decision-making, organizational flexibility and competition , until now virtually non-existent; In short, what tends is to transform the public hospital into a hospital of self-management. The new trends in administration need to consider some principles to be taken into account in the construction of the new model of hospital organization, namely:
Flat, participatory structures, co -responsible for the management.
Participation of citizens, integrating different social organizations to do hospital work.
Self-management of establishments, granting them the faculties so that they can adequately assume the responsibilities they are responsible for.
Flexible structures, easy to adapt to the changes, avoiding the segmentation and creation of clinical services of specialties that stiffen the structure and resources.
Undifferentiated resources, of multiple uses, organized by complexity, concentrating scarce resources, such as critical patient units.
Poly-functionality of the resource
Processes of short or minimum duration, tending to the ambulatory care, which leads us to give the utmost importance to socio-health care and continuity of care.
Development of human resources; have the support instances that allow to have a healthy, trained and motivated human resource. This implies contemplating the functions of well-being, training, risk prevention, occupational health, among others.
Integration and coordination with the network, especially the Hospital with the primary level of care.
The framework for moving from this traditional model based on a purely operational management to this new model of hospital management based on strategic planning and control, is the Balanced Scorecard, which we present below.
Administrative matrix to manage hospitals
For the purposes of developing an administrative matrix or scorecard to manage hospitals, the following scheme suggested by Ostengo (2006) is presented below:
Strategic planning:
It is a process to diagram the strategy. To plan is to think about the future, it is an activity that has supremacy in the administrative process, and necessarily is of a prospective nature. It is designed by senior management, involved in the fulfillment of medium and long-term organizational objectives. Involves the declaration of a mission, the establishment of global objectives and the determination of strategies through the formulation of plans and the setting of policies.
Management control
It is the process by which the development of the most appropriate strategy to carry out the activities is guaranteed. To carry out this control, we have a strategic management tool called the Integral Control Panel (CMI). "The CMI is a tool that allows monitoring through indicators (financial, operational, human resources, quality, etc.) compliance with the strategy developed by management, while allowing quick and accurate decisions to achieve the objectives" (De Marco and Medina, 2012, p. 4).
As expressed by the authors Kaplan and Norton (2002), the CMI is a tool that allows the monitoring of organizational objectives, through the systematic visualization of the deviations of the most critical variables, facilitating the correction of the strategies and control. This CMI translates the strategy and mission of an organization into a set of indicators from four balanced perspectives: finances, patients, internal processes, and training and growth. These four perspectives are interrelated and should always be analyzed together, making it clear that the action in any of these perspectives will probably have an impact on the others. This causal relationship between the different perspectives is carried out through the so-called strategic map, which aims to achieve a better articulation between the strategic definitions and the set of indicators in the scorecard.
Performance evaluation
No strategy can be effectively implemented if it does not have an appropriate methodology to measure management performance. For this purpose, it is considered convenient to prepare a work paper that reveals this analysis and is known as the Control Board, which allows analyzing, individually and together, the financial and non-financial indicators of the organization, through a weighting method In the Control Panel the information provided by the different indicators used must be compared with the pre-established goals by the organization in order to analyze the variations that have occurred and adopt the corrective measures. One method to qualify these variations and interpret them easily is the semaphore method, in which the colors green, yellow, red and black are used to qualify the variation of each indicator.
Definition of variables and indicators
The integral management of an organization implies the balanced and total measurement of financial management and intangible management.
In this sense, the integral management of a Hospital should not only be limited to the financial economic, but should be involved in the social, human, ethical and environmental, among others. In order to achieve this, the Hospital must administer information related / related to the daily work of the Hospital in its interaction with society, which exceeds that arising from the account surrenders that reflect the income and expenses.
Thus, the variables and indicators to be considered in the balanced scorecard can be classified into two types: variables and financial indicators and variables and non-financial indicators.
The financial indicators arise from the accounting information system, and are in historical or budgeted figures or pesos.
The non-financial indicators are those that arise from the managerial information system and can be in figures or weights, numbers or directly descriptions; These non-financial indicators allow us to measure the achievement of certain competitive advantages, which come today from the creation of value, through the management of intangible capital, which can be represented through the following scheme, in which it can be seen as the Value creation process is measured from different perspectives, namely:
1. Intangible assets: must be aligned with the strategy of creating value
This perspective constitutes the starting point of any lasting and sustainable change. Identifies and analyzes the most important intangibles of the organization, they are: the intellectual capital or Human Resources, the informational capital and the organizational culture.
2. Internal processes: create value for patients and the hospital
This perspective identifies the critical processes that have the greatest impact with the strategy and that define the value chain of the processes. They are process of service management, patient management process, innovation process, and regulatory and social processes.
3. Perspective of the patient: creates the differentiated and sustainable value
This perspective is related to what the patient values in the provision of the service offered by the institution. It is the core of the execution of the strategy. To analyze this perspective, three aspects were considered: image and prestige of the service, attributes or quality of the service, and relations with the patient.
4. The financial perspective: provides the tangible definition of value
This perspective describes the tangible results of the strategy in terms of financial results, and aims to guarantee sufficiency and financial sustainability, creating in turn economic value for the institution in terms of internal growth. Within this approach we must consider: the income growth strategy and the productivity strategy.
The union of all these pieces represents a strategic map that represents how the hospital creates value.
Finally, everything that has been done makes sense if the strategy is translated into a set of representative indicators, in order to create the control panel that will allow knowing if the institution is heading in the desired direction.
Universe of analysis
In the province of Tucumán, there is the Ministry of Public Health, dependent on the Executive Branch, of this ministry depends the Provincial Health System (SIPROSA), which has as president the Minister of Health. The SIPROSA regulates the activity of the assistance centers of Tucumán. For this the province is divided sanitarily into four programmatic areas: East, West, Center and South. In turn, each program area is divided into operational areas, each of which has a Reference Node Hospital and Primary Health Care Centers (CAPS) that are operationally dependent on that hospital.
We will find particularities such as the fact that hospitals, depending on a higher body that regulates all hospitals and health centers: SIPROSA, cannot make all decisions as independent organizations, but must respect the decisions of that regulatory entity, for example in acquisition of materials and medicines, incorporation of human resources, salaries, etc.
In this particular case, our universe of analysis will focus on the Hospital Ángel C. Padilla. It is a hospital for adult patients, it is polyvalent and highly complex; It is located in the capital of the province of Tucumán. It is dedicated to the care of critical patients with acute pathologies. It is the provincial and regional reference center, integrated to the network of providers of the Provincial Health System, under the Ministry of Public Health of Tucumán. It is a school hospital, trainer and motivator of professionals.
Indicators of the Internment Area
De Marco and Medina (2012) propose a series of indicators to measure the productivity of hospitals. Within this framework, indicators referring to the hospitalization area corresponding to the 2007-2011 period in the analyzed hospital are presented below.
Performance indicators and mortality rate
Average daily bed available
Available beds are the number of beds installed in the hospital in conditions of use, for the care of hospitalized patients, regardless of whether they are occupied or not. This number may vary daily due to the addition of beds due to seasonal demand, emergency, etc., or the removal of beds for repair, disinfection, painting of the premises, temporary closure of the service, etc.
The available bedtime is the period from 0 to 24 hours a day, during which a hospital bed is kept available for the use of hospitalized patients. The total available days-beds of the period are obtained from the Daily Census.
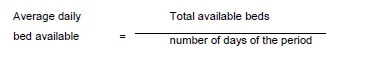
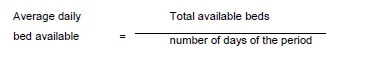
The average daily bed available is the number of beds that are available on average daily. It is obtained by dividing the total available days-beds during a period by the number of days of the period.
Average daily patient day
The hospitality or patient day is the set of services provided to a hospitalized patient during the period between 0 and 24 hours of a central day. That is to say, the care given daily to each hospitalized patient is counted as a patient day (a hospitality). The case of a patient who ingresses and withdraws on the same day, will be committed as a patient day. The total number of days of a period was obtained by adding the daily number of patient days of that period.
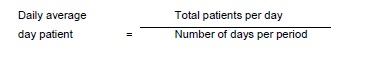
The average daily patient day is the average number of hospitalized patients receiving daily care during a period. It is obtained by dividing the total number of day patients during a period by the total days of that period.
Percentage of occupation
It is the percentage of beds that on average were occupied daily during the period. It is obtained by dividing the total number of patients per day of the period by the total available days-beds of the period and multiplying by 100.
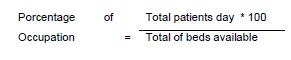
Total patients day: is the number of inpatients who are treated during the month. Adding day to day during the month
Total available beds: is the number of beds available in the hospital during the month, those that are occupied and the unoccupied that are in good condition. If the total of available beds of the month is divided into the days that you have each month you get a Daily Average of Available Beds. It is calculated by adding day by day.
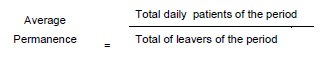
Average permanence
It is the number of days that on average each patient left during a period has remained interned. It is obtained by dividing the sum of days of stay of the patients graduated in a period by the number of discharges of the period. In general acute care establishments, this indicator should not exceed the maximum of 10 days.
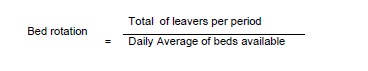
Bed rotation
It is a measure of bed utilization that indicates the number of patients who leave each bed during a period. It is obtained by dividing the number of leavers by the average of available beds during a period. The data for its calculation are obtained from the Daily Census.
It is the average rotation of the beds and expresses how many patients spend in a given period on average per available bed. The optimal measure for this type of indicator should range from 3 to 4 patients approximately per month.
Mortality Rate
Any decrease in the mortality rate implies an improvement in the quality of the service.
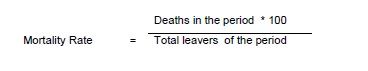
Deaths Period: includes the deaths that occurred in a given period.
Total period discharges: is the number of patients who leave the hospital, either because they are discharged or due to deaths in the period.
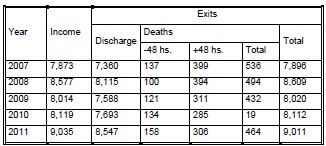
Table N°: 1: Total beds available, patient day, expenses, performance indicators and mortality rate per year Padilla Hospital - Period 2007-2011
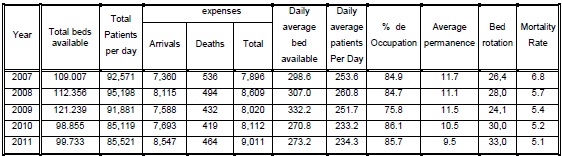
Source: Statistics Department Hospital Padilla – Statistics Summary years 2007-2011
From the statistical analysis of the activities carried out in the Hospital, based on the information of the hospitalization area provided by the hospital authorities, it appears that in the hospitalization area a daily average of 296 beds was used in the period 2007 - 2011 This average is affected by the refurbishing that is periodically carried out in the rooms according to the needs, in which a sector is temporarily closed, part of another sector is occupied, another is reopened, and so on.
Within this sector, in order for the occupation to be optimal, it should reach 80%, given that 20% must always be reserved in case of catastrophes. This percentage calculated on a global level is fulfilled, but taking by service it is found that in some cases the occupation reaches a level of 100% as for example the rooms of Neurosurgery and Gynecology, while in others the occupation is below the optimal level.
It is observed that in the period analyzed (except for the year 2009) the percentage of global occupation does not vary significantly, oscillating by 85%. In 2009, it reached 75%, below the optimum level, which is due to the continuous stoppages of services, as well as to the remodeling of infrastructure carried out in the hospital.
If the bed rotation is analyzed taking as a parameter the whole year, the same to reach its optimum level should be between 36 and 48 leavers per bed. However, in the years analyzed, the Hospital is below it, highlighting that in 2009 it reached its maximum rotation decrease, reaching 24 times that the bed is used per year. Some of the reasons that caused this situation were due to the continuous strikes as well as the closing of rooms for remodeling, a situation that has an impact on the average stay, which we can see is above the standard (in general establishments of acute illnesses, this indicator should not exceed the maximum of 10 days).
In turn, said average is affected by the delay in the provision of auxiliary services, such as tomography, x-rays, prosthetic supplies, among others.
Among the services that generally have high turnover are surgery, rheumatology, and shifts, while among the services with less turnover are medical clinic, gastroenterology and traumatology.
In the years 2010 and 2011 a decrease in the time of stay of the patients began to be observed, parallel to an increase in the rotation of the beds and in the percentage of occupation, consequence of a more effective and efficient provision of the services in Hospital.
With regard to the mortality rate, it is noted that between 2007 and 2011, there was a decrease in it to reach 5%. One of the factors that led to this improvement was the change in infrastructure as well as the new technological equipment used in the different services. In this sense it is necessary to mention the great progress that medicine has made in recent years with methods for the detection and management of diseases, in addition to the improvement of measures to prevent the disease; As a result, mortality rates have decreased in most of the public hospitals in the province.
This group of indicators allows the Hospital Management:
- Know the variations in the number of beds available during a period, which is a dynamic element since it involves all the resources available to the hospital to care for their patients, from the medical ability to attend to the last necessary material component . Therefore, the hospital beds are related to the capacity of the Hospital's medical services as well as administrative support.
- Estimate the potential annual demand for hospital beds for the purpose of budget preparation.
- The average length of stay serves to assess the degree of use of hospital beds and indirectly the quality of services, since excessive hospitalization times may reflect, among other causes, technical deficiencies. The days of internment vary according to the pathologies and specialties, so this indicator has little utility when you want to measure the average permanence of the hospitalized group. Its real utility is in the calculation for services or specialties.
- Evaluate and take corrective measures to avoid prolonged stays, beyond what is acceptable, which may be due to inadequate diagnosis or treatment, patients under study, patients receiving physiotherapy, rehabilitation or radiotherapy services, inefficiency of support services (radiology, laboratory, etc.), problems of organization in medical work and / or delays in the supply of medicines to the room.
- By means of the occupation percentage it is possible to establish plans for the maximum use of hospital beds; know the services where the use of the beds is excessive or insufficient; maintain the optimum occupation ratio; improve the distribution of beds between the different services and adapt the facilities to the needs of the hospital. This percentage is modified in relation to the size of the hospital: in a hospital with a few beds, an income increases it considerably, while in one of many beds it hardly changes it. That is why it is convenient to calculate the percentages of occupation for each service or specialty.
- Adopt the necessary measures to correct the factors that may alter the occupation percentage, such as: unnecessary income, insufficient or excessive number of beds, slow recovery for inadequate treatments, and / or for delays in discharge for social or administrative reasons. - Evaluate bed performance, either in general for the entire hospital or for a service or specialty.
- Know the distribution of hospital beds between services or specialties, with respect to the total available hospital beds. It provides information on the distribution of available beds, which does not always coincide with the demand. For this reason, it is convenient to relate this indicator with the results of the period of permanence, rotation of bed and percentage of occupation of beds, which indicate the pressure of the demand, to achieve a better appreciation of the efficient use of the bed resource.
-Adequate use of resources for the care of hospitalized patients and assess the importance given to diagnostic and / or treatment services.
- The mortality rate provides an idea of the quality of care provided to hospitalized patients, allowing a higher level of accuracy, since it is presumed that the deaths occurred are associated with hospital care. It can be applied in general or to services or specialties.
Number of admissions and leavings by hospitalization sector
Admissions
It is the entry of a person to the hospital as an inpatient. All admission to the hospital involves the occupation of a hospital bed.
In order to record the admission, the following must be taken into account:
- Only one admission should be posted for each patient during the period that he / she is hospitalized. A patient who leaves the hospital and is re-admitted for the same process constitutes a new admission.
- In the event that a hospitalized patient is transferred to another service different from the one entered, it should be considered as a transfer and not as a second income.
- Hospitalized patients, at the beginning of a new year, should be counted as the existence of hospitalized patients in the year prior to the one being started and not as new income.
Leaving
It is the exit of the establishment of a hospitable patient. A discharge always implies the conclusion of the period of hospitalization and the vacancy of a hospital bed, either by leaving or by death.
A differentiation was also established between the mortality of + 48 hours and from 48 hours, considering the mortality of - 48 hours was not the responsibility of the hospital given the conditions in which the patient entered. Not so with the mortality of + 48 hours which depended on the efficiency of the service provided by the hospital
Table Nº 2: Number of incomes and exits – Hospital Padilla – Períod 2007-2011
Source: Statistics Department Hospital Padilla – Statistics Summary years 2007-2011
Regarding the amount of income and expenses recorded in the hospitalization area in the period under study, an increase in the number of admissions and discharges due to medical discharges is generally observed, which coincides with the increase in bed turnover, and the decrease in the average length of stay of patients and the death rate indicated in the preceding paragraphs. The main diagnoses of discharges were: vesicular lithiasis, polytraumatisms, cerebrovascular accident, rheumatoid arthritis, fractures in the lower limb, appendicitis and suicide attempts. It also warns that in 2009 there were 7% less outlays than the year 2008 in this area; between June and September of that year, the rheumatology sector was closed and the same beds were fitted for the hospitalization of patients with influenza-like illnesses (ETI), from where 64 discharges occurred.
This group of indicators allows the Hospital Management:
- To know the trend in the movement of patient income and exits, globally for the entire hospital and hospitalization sector, in order to allocate the necessary physical, technological and human resources to cover the needs of the hospital in a timely manner for the users.
- To evaluate the productivity and efficiency of each of the hospitalization sectors, which will allow having an idea of the quality of care.
-To establish the causes of mortality of + 48 hours, which is generally related to the resolution capacity of the institution in terms of opportunity, technical-scientific rationality and comprehensive care.
- Evaluate the degree of use of beds in the emergency service. Theoretically, an emergency bed should not be occupied for more than 24 hours; however, in most hospitals the length of stay exceeds this period, which may be due to technical deficiencies or the lack of available beds in hospitalization services.
- To have an idea of the degree of use of the beds in a given period in a global manner and by service, by means of the existing relationship between the patients who enter and the actual capacity of the hospital beds, in order to establish plans for the use maximum of the beds, to know if the use of the beds is excessive or insufficient, to maintain the optimum proportion of occupation, and to adapt the facilities to the needs of the service.
- Establish the resolute capacity of the hospitalization service in relation to the type of pathology that is attended, and also to establish the causes for which a patient is transferred to another healthcare center. This information will allow identifying the corrective measures that must be carried out to improve the service.
Percentage of hospital infection
This indicator relates the number of patients who presented nosocomial infections during their hospital stay with the total number of discharges during the period. It reflects the efficiency in the treatment of patients and the care dedicated to them. The smaller the measure, the higher the quality and prestige, which results in a greater rotation of the beds and a decrease in operating costs.
With regard to the causes of hospital infection, these can come from:
In-hospital infection (IH)
Catheter-associated bacteremia infection (CAI)
Respirator-associated infection (IAR)
Infection associated with bladder catheter (IASV)
According to the control panel of epidemiological surveillance corresponding to the period 2007 - 2011, in the HACP the following percentages of hospital infection were registered:
Table Nº 3: Hospital Infections – Hospital Padilla – Períod 2007-2011
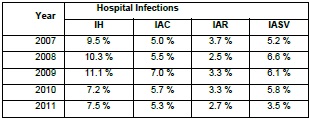
Source: Statistics Department Hospital Padilla – Statistics Summary years 2007-2011
As can be seen, in general there was a decrease in the value of this indicator in the period analyzed.
Percentage of unscheduled readmissions
This indicator is intended to evaluate the number of patients re-admitted to the hospital within 72 hours of discharge with the same diagnosis or diagnosis of a higher category. The untimely nature of an unplanned re-entry presupposes the existence of processes that are not detected or adequately assessed, which generate a negative impact on the patient.
According to information provided by the Admission Section of the HACP Internment Rooms, the number of readmissions registered annually in the 2007-2011 period were:
Tabla Nº 4: Non Programmed Readmissions– Hospital Padilla – Período 2007-2011
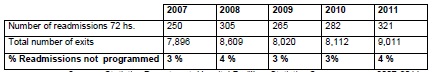
Source: Statistics Department Hospital Padilla – Statistics Summary years 2007-2011
Paramedics on the number of beds
It is an indicator of availability, in this case, of paramedics (staff category composed mainly of nurses). It is assumed that as the index increases, there will be greater availability of the personnel in question. Obviously, an excessive increase can be dysfunctional and, therefore, the indicator should be complemented with those referring to the costs of providing the services.
According to data released in December 2011, the HACP has 298 nurses.
With regard to the number of beds, the capacity of the Hospital is 375 beds per day distributed in 16 inpatient rooms; this amount of beds may vary due to refurbishing, temporary needs, etc.
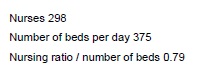
Based on this indicator, the number of nurses for each available bed is less than one.
Doctors re the number of beds
This indicator has the same reasoning as the previous one but for doctors. According to data released in December 2011, the HACP has 281 doctors.
Based on this indicator, the number of doctors for each available bed is less than one.
Control Room of the Internment Area
The results are the end of the road, which must be in line with the vision of the institution, its mission, strategic and operational planning. To make an adequate follow-up of the fulfillment of objectives, goals and results, it is necessary to elaborate indicators.
If we take into account that when managing human and physical resources used, and that the objectives of the Hospital are to increase productivity with quality, satisfying the internal and external client and achieving adequate results, the indicators should measure these dimensions: human resource, physical, financial, processes that allow to improve the productivity and the opinion of the user.
A priori the integral control panel of a public hospital can appear as a complex structure and difficult to carry out. However, the experiences show that if it responds to the needs of the hospital and the steps for its implementation are followed, it can be carried out with relative effort.
The set of indicators must respond to the needs of the institution, that is why it is key in the choice of indicators to be clear that we are measuring, its importance, cost and feasibility of its collection and maintenance over time.
Taking into account these premises, the Directorate to measure the performance of the hospitalization area, recognized on this board the process indicators, understanding that their monitoring allows to perform tasks of prevention and continuous improvement.
The elaboration of a control panel for the hospitalization area, turned out to be an excellent experience, for the work of reflection and previous analysis that its preparation required. The chosen indicators, the proposed objectives and the weighting factors established for each one were the result of consensus between the Directorate and the Service and Departmental Heads based on the availability of the information, its cost and feasibility of collection, and the declaration of the mission and global goals previously defined, which has the function to serve as a guide for the action, and therefore, it must be known and understood by all levels of the organization.
At this point, it is convenient to differentiate what is a declaration of purposes as a document, from what is the use of it as a management tool. The Management must be the first committed to the described ideal, because it is it which must show the way and motivate the other members to achieve the desired change day by day, leading to action what a priori seems a vague enunciation of desires.
For its part, the strategic map and the Integral Scorecard are intended to collaborate with the concretion of the wishes and goals stated above. In particular, the WCC allows presenting the reality of the institution at a specific moment, as if it were a radiographic plate, where it is possible to identify the symptoms of organizational diseases in order to attack their causes.
This set of developed indicators does not solve the problems, but it allows quickly knowing deviations in the proposed goals, as well as constituting an excellent tool for quality management.
The following table shows the control panel of the Hospital's hospitalization area, based on the indicators presented in this work, corresponding to the year 2011.
Table Nº 5: Internation Command Chart – Hospital Padilla – Año 2011
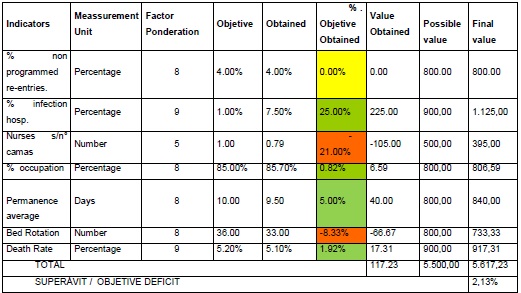
Source: Own Elaboration
Details of the Control Panel columns:
1. INDICATORS: the algorithm of indicators is written on it.
2. PONDERATION FACTOR: determined at the beginning of the period under study, according to the importance that the activity has for the organization. It can be done through a scale of 1 to 10, the greater the problem the greater the ponderation factor.
3. OBJECTIVE: is what you want to achieve in the activity considered. It must be quantifiable, realistic, and feasible to reach in the period and can be expressed in percentage, absolute number, pesos, etc.
4. RESULT OBTAINED: is the result reached at the end of the period.
5.% COMPLIANCE OF THE OBJECTIVE: it is obtained as follows:
[(Objective (col 3) - Rtdo Obtained (col 4) / Objective (col.3)] x 100
This difference can be positive, if the goal was overcome or negative, if it was not reached. In some cases there are variables that are valence contrary to the others, therefore when the result is higher than the goal, it yields a negative value.
6. VALUE OBTAINED: it arises from multiplying the% of compliance with the objective by the weighting factor, that is, it arises from: column 5 x column 2.
This is in order to give a relative value to the final result, that is, it converts the resulting one into more positive points or more negative points.
7. POSSIBLE VALUE: it is achieved by multiplying the ponderation factor by 100, which would be the maximum to obtain if the goal were met in a total way.
8. FINAL VALUE: is obtained by adding or subtracting the Result Obtained from the Possible Result and it will give points above or below the goal. With these accumulated data, it will be possible to know the surplus or social deficit of the decisions. When the sum of the points of the Final Result is greater than that of the Possible Results, the actions proposed by the company have been satisfactorily fulfilled. When said amount is lower, it will not have been possible to comply with them.
From the analysis of the results obtained in each of the indicators raised in the scorecard throughout the period, and the objectives indicated for each of them, it appears that in general the Hospital has satisfactorily fulfilled the proposed actions in the area of hospitalization for the year 2011.
This can be seen visually through the number of indicators that met the standard within the acceptable range (marked with green) as well as that indicator that although met the objective it is necessary to take minor corrective actions and be aware of the same (indicated with yellow color), while the indicators marked with red color are those that did not comply with the guidelines established for the period analyzed and therefore require urgent actions in those areas to improve them.
CONCLUSION
A matrix of management indicators to administer hospitals is a practical guide that allows to present the reality of the institution at a specific moment, a radiographic plate, where it is possible to identify the symptoms of organizational diseases in order to attack their causes, to the time that it will allow managers to know if the institution is directed towards the final achievement of its goal.
The indicators proposed by the business administration are used by hospital institutions to improve the management of the health service, thus achieving a more efficient system.
The construction of indicators for the rational use of resources requires as a central action the training of the human capital of the Hospital in the administrative - accounting knowledge.
Although this instrument will not solve the problems that the hospital faces on a daily basis, it will be of great help if it is applied correctly because it will allow it to react, carry out and disseminate a strategy change if necessary, becoming an important quality management tool
BIBLIOGRAPHCIAL ABSTRACT
Please refer to articles Spanish Biographical abstract.
REFERENCES
Please refer to articles in Spanish Bibliography.